Once upon a time, no one understood tinnitus. People thought it was a hallucination and indication of mental health issue. No help was available. People resorted to ‘distract themselves’ in their own ways, rather than going to a healer. This was some time ago!
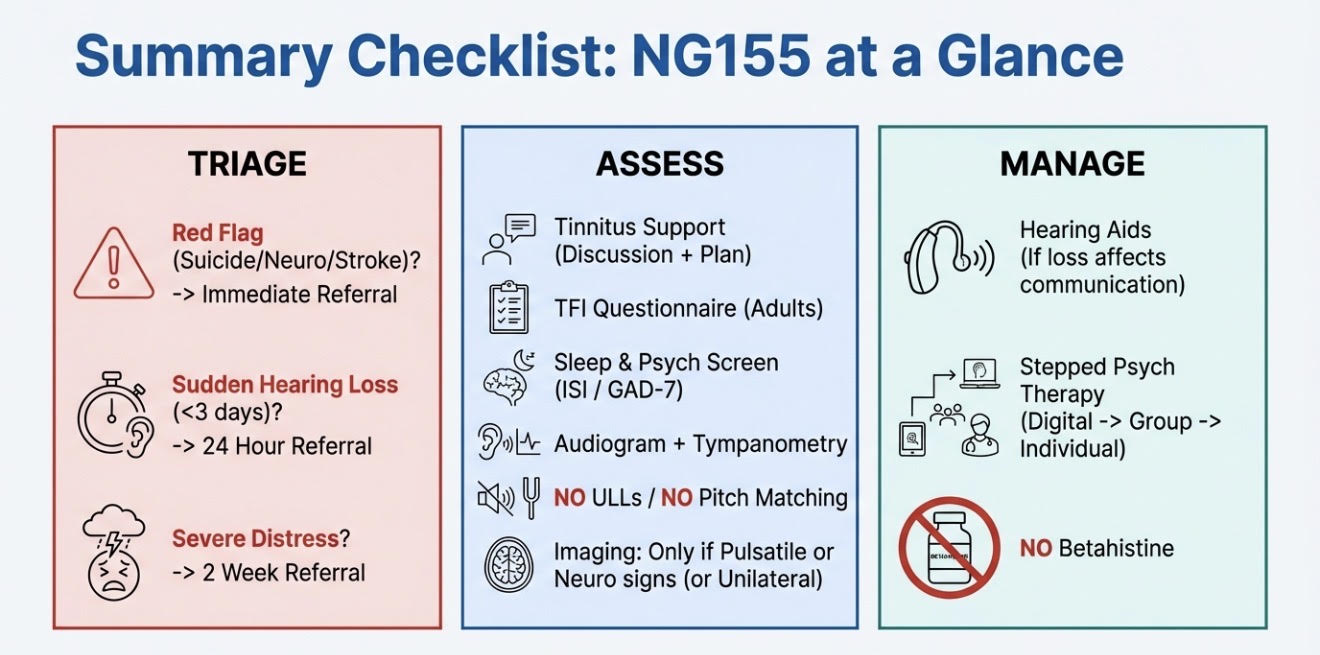
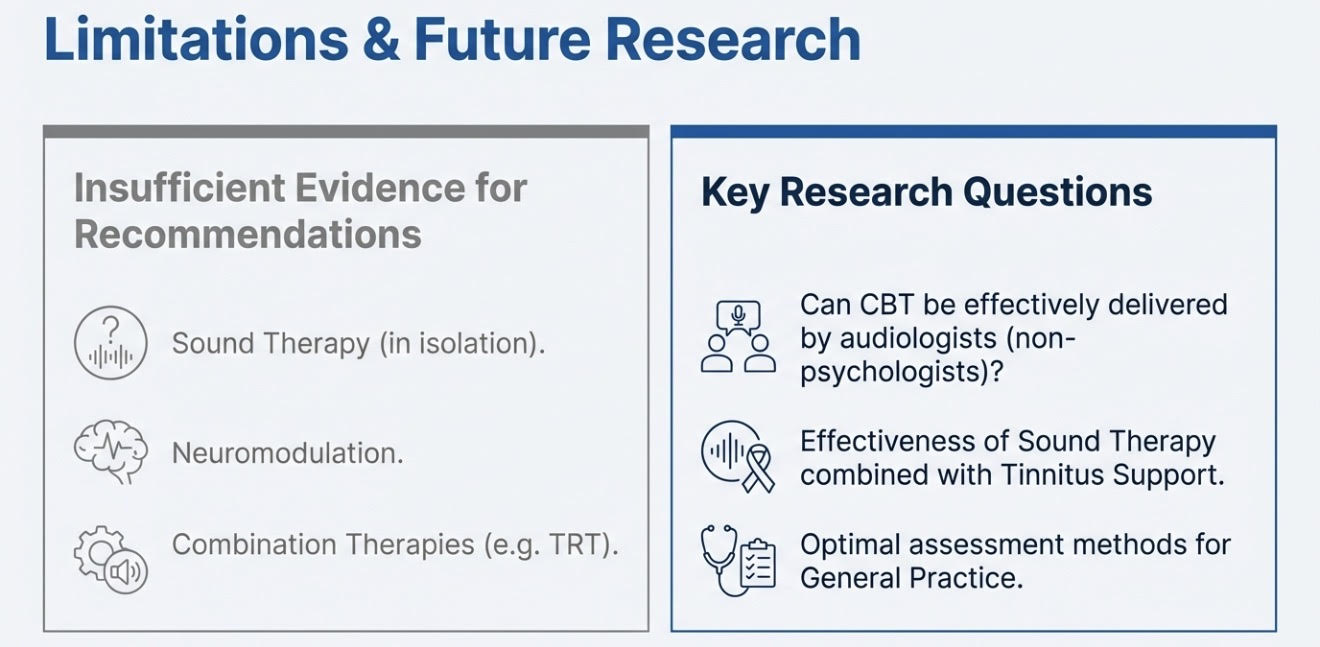
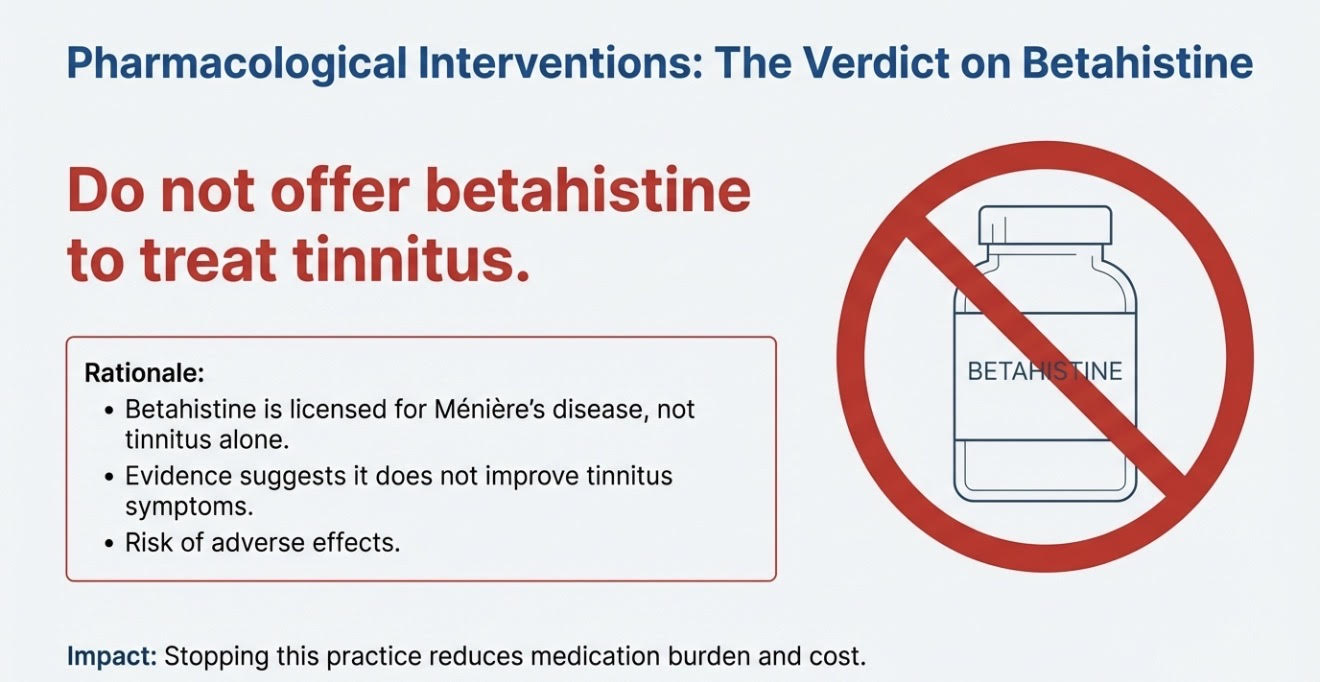
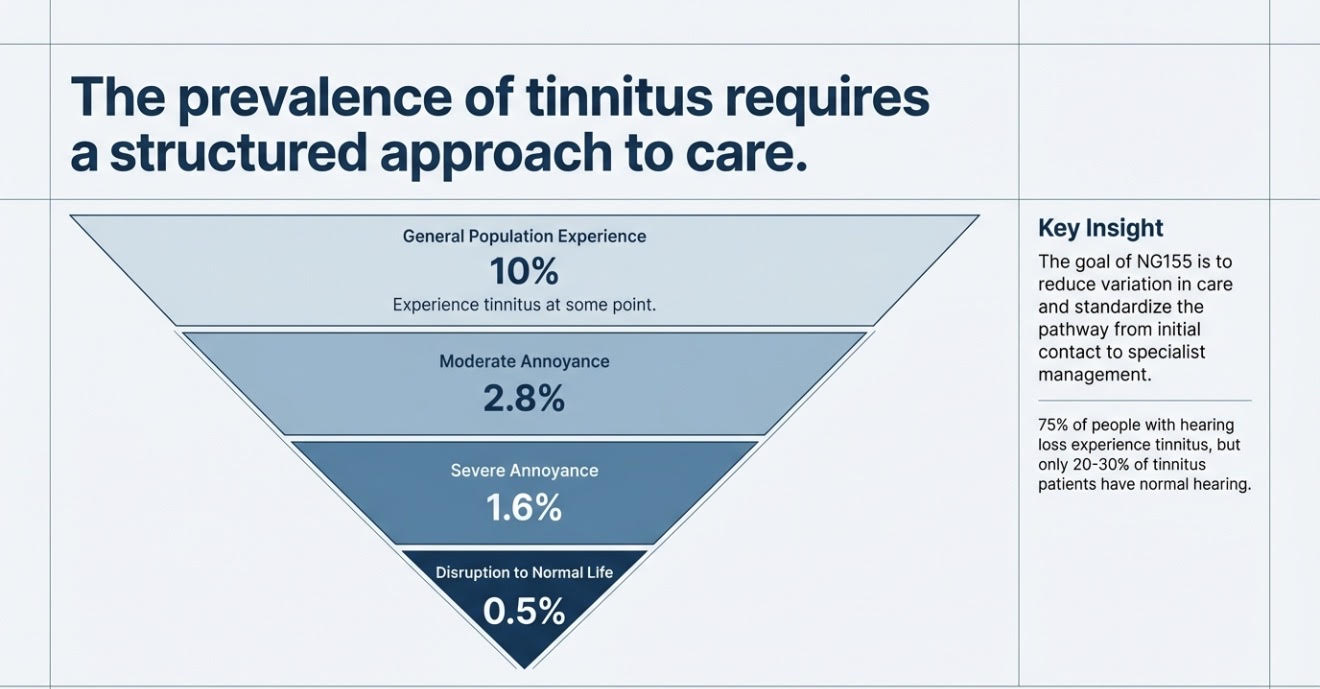
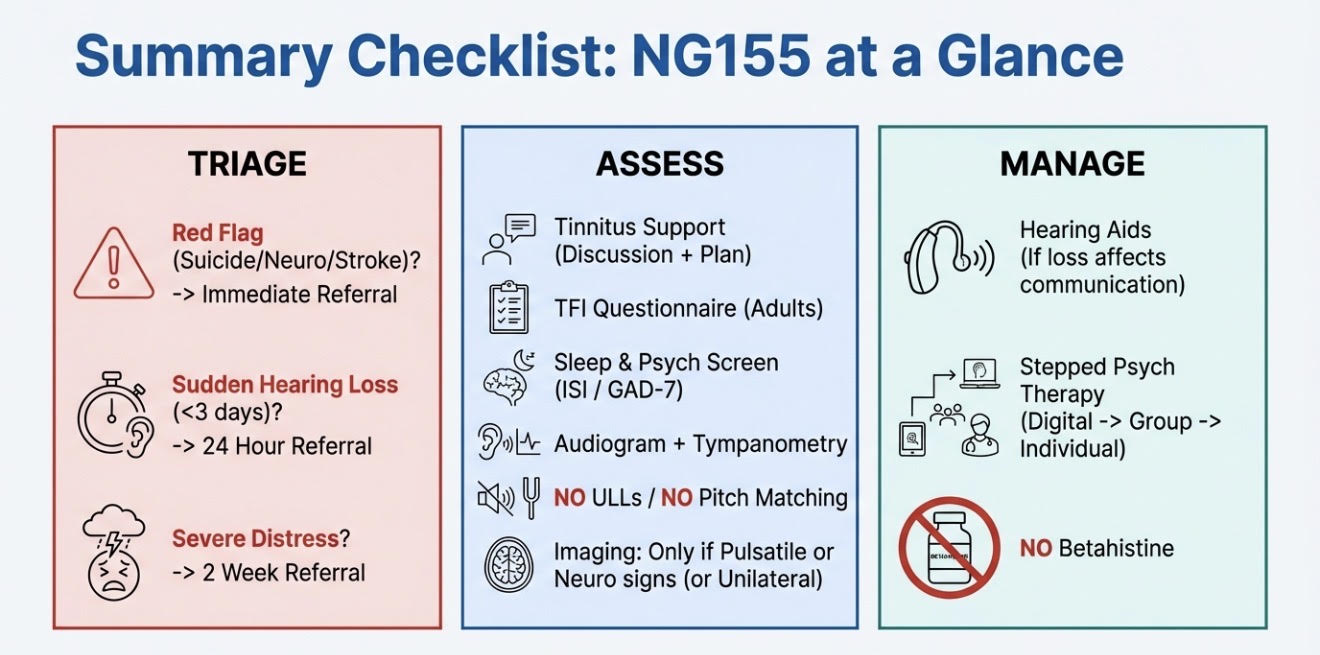
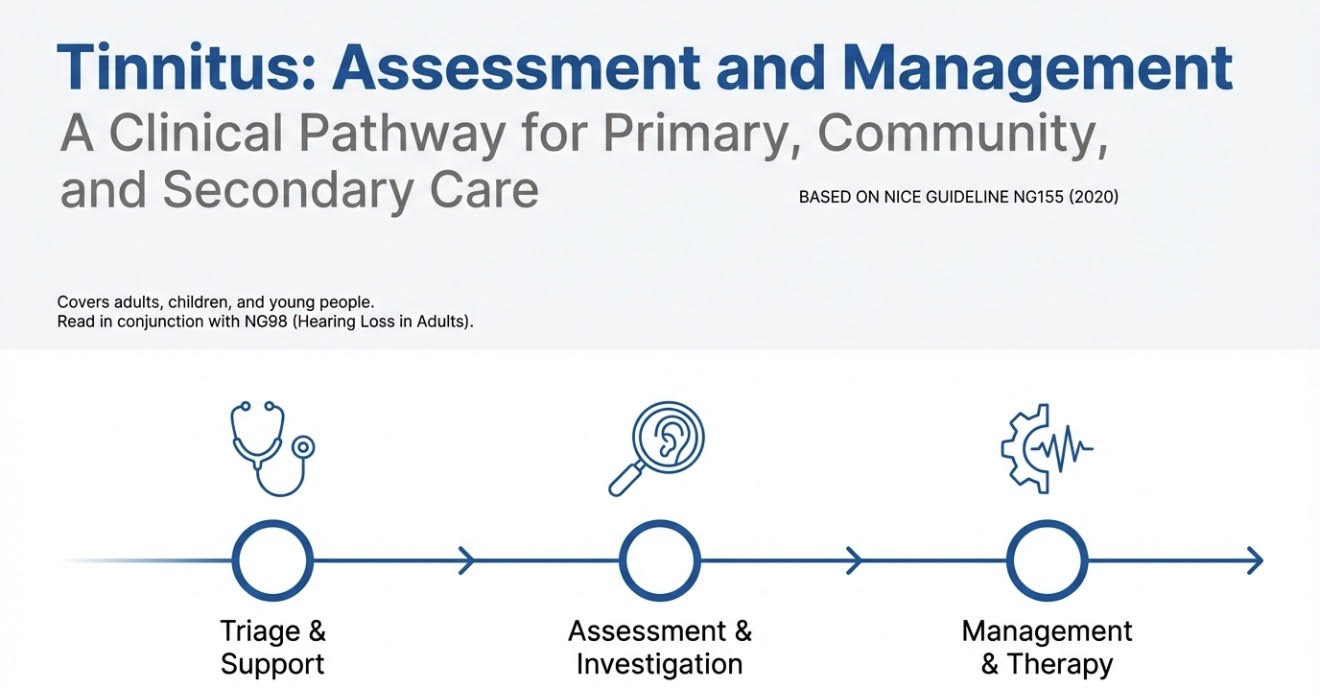
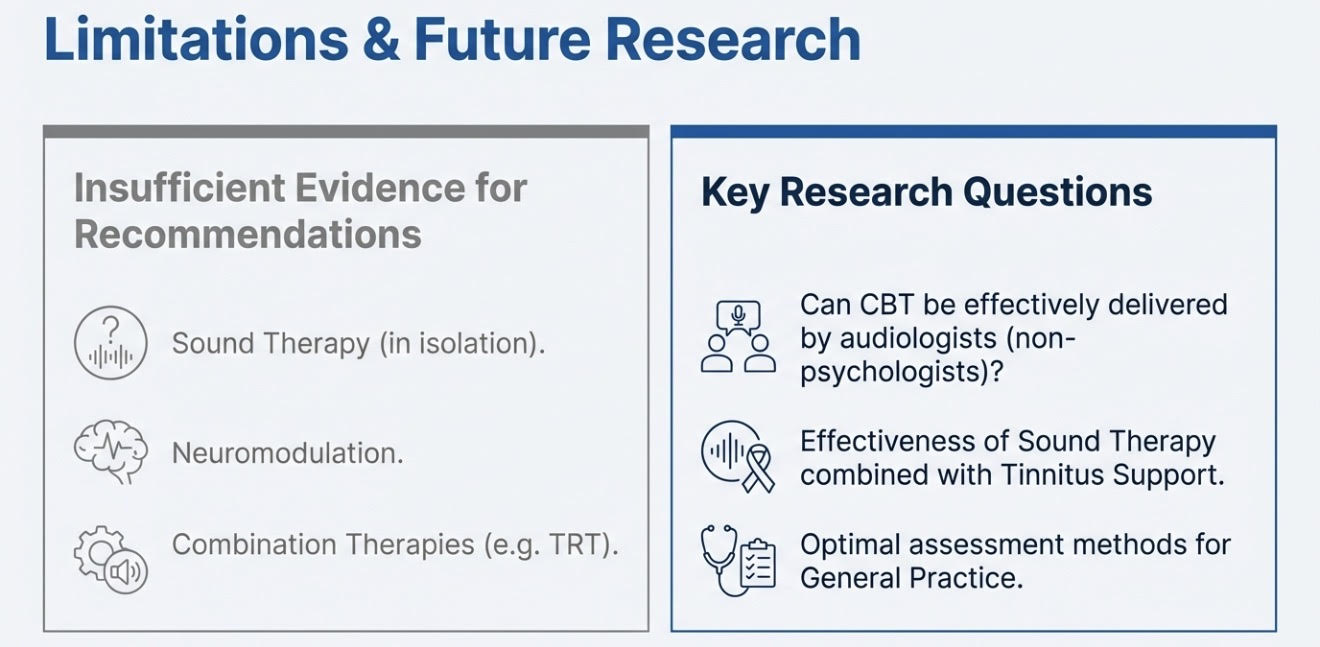
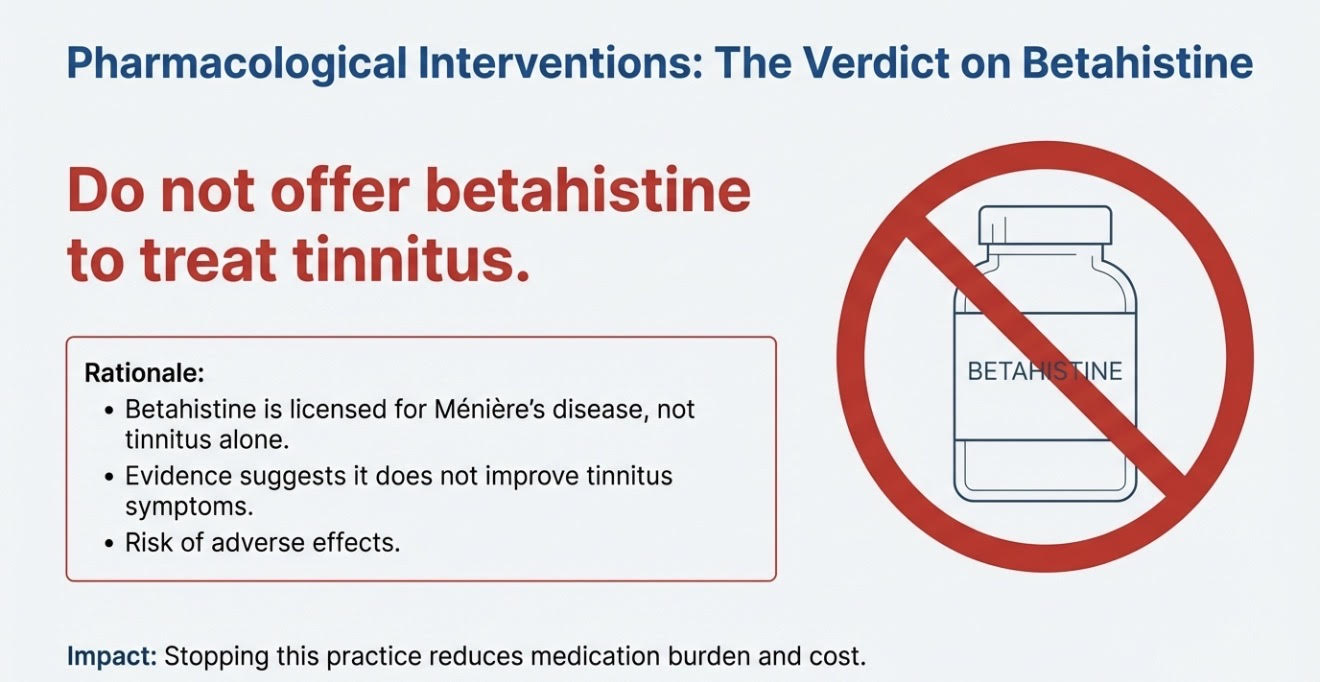
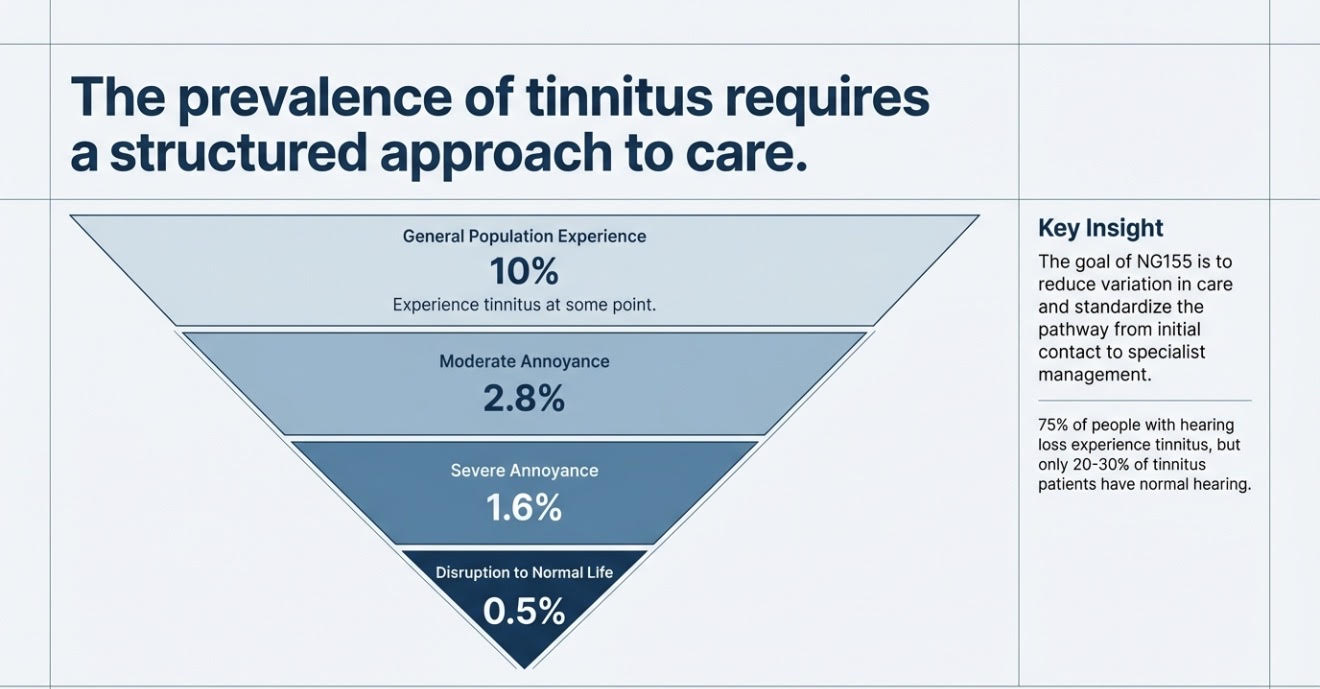
Things have supposed to change because it is 21st century. We know much more about physical, emotional and mental health. There is a body of peer-review evidence on what tinnitus is and isn’t, what you should and should not do. We even have a guidance from National Institute of Clinical Excellence, if you don’t have the time or will to do your own research https://www.nice.org.uk/guidance/ng155
So, times have changed or they should have!
I recently saw a young patient who had first presented with tinnitus about a couple of years ago to 3-4 healthcare professionals. Standard audiology testing was satisfactory at the time. I am sure it was very well-meaning advice, but she was essentially told to try to ‘distract herself’ from the tinnitus.
Imagine having a toothache that’s keeping you up at night, and the dentist tells you to distract yourself from it. Or being in the middle of an anxiety attack and someone says, “Just ignore it.” Or telling someone with asthma to put on some soothing music and try not to focus on the wheezing. It sounds absurd — because the symptom is real. It needs understanding and management, not dismissal.
Tinnitus is no different.
Anyways, coming back to our young patient- two years down the line, with a lack of proper information from her healthcare professionals, she turned to Dr Google. She got pulled into late-night tinnitus forums that painted a very doom-and-gloom picture about the outlook. Because of the perception she had already developed, she absorbed the negative feedback more strongly- sucked deeper into the vortex of spiralling negative thoughts!
What I often find is that online feedback about tinnitus management is skewed. Many of the people who improve significantly do not go back and write about their experience. Those who are still struggling are more likely to post. I mean, I have not encountered much positive feedback online, which is contrary to the clinical experience. We know that many people benefit from proper, structured approaches — but that positive side is underrepresented online.
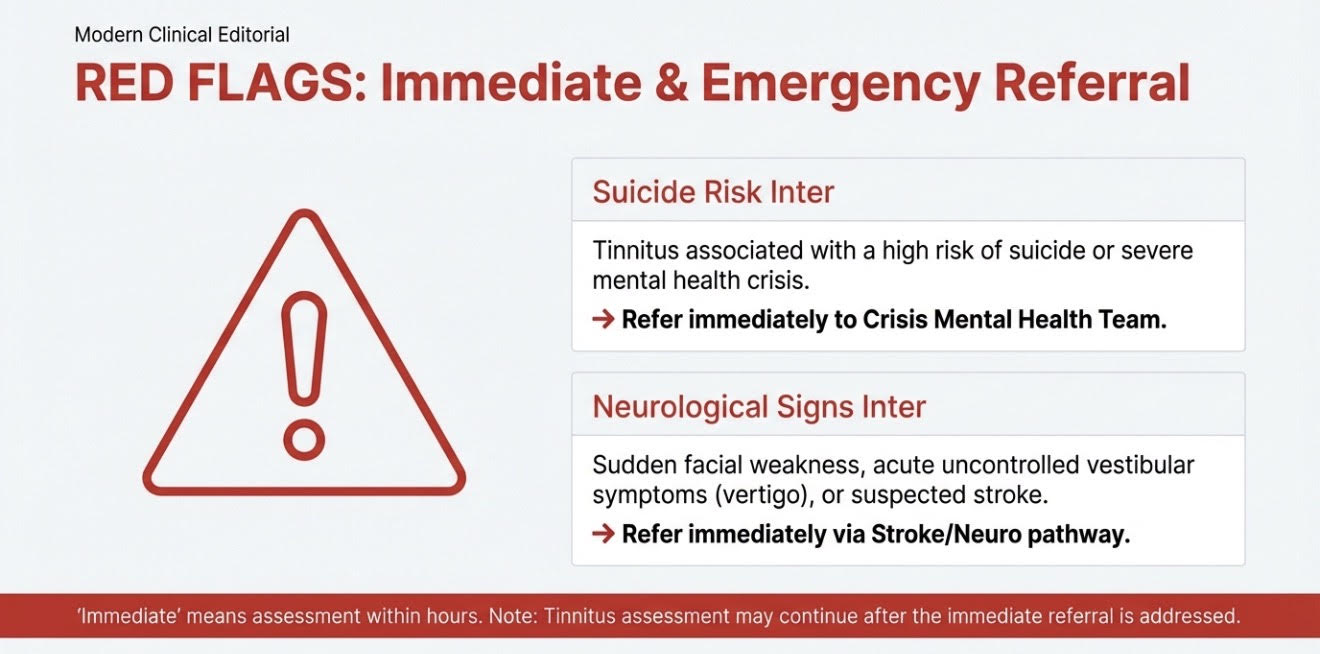
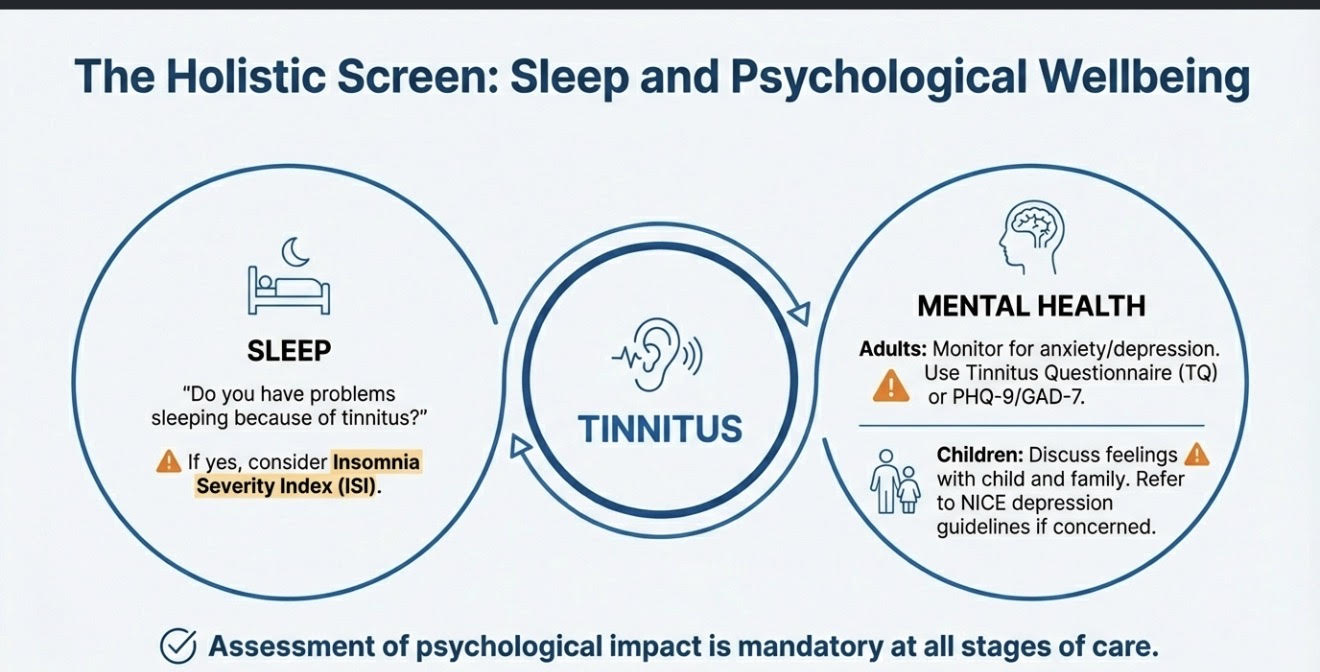
By the time she came to see me, she was completely devastated. Tinnitus had taken over her life. It was affecting her work. She felt helpless and dejected. She had even considered taking a sabbatical. Despite everything, she decided to put her faith in another healthcare professional and seek help one more time.
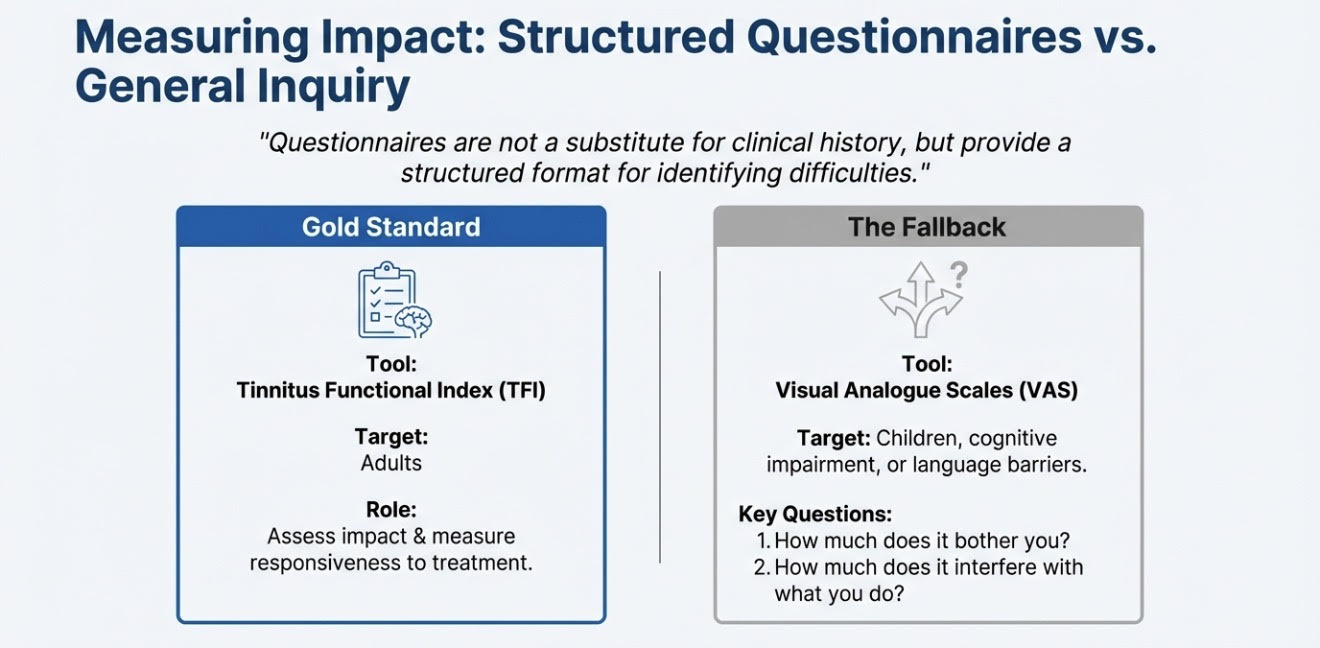
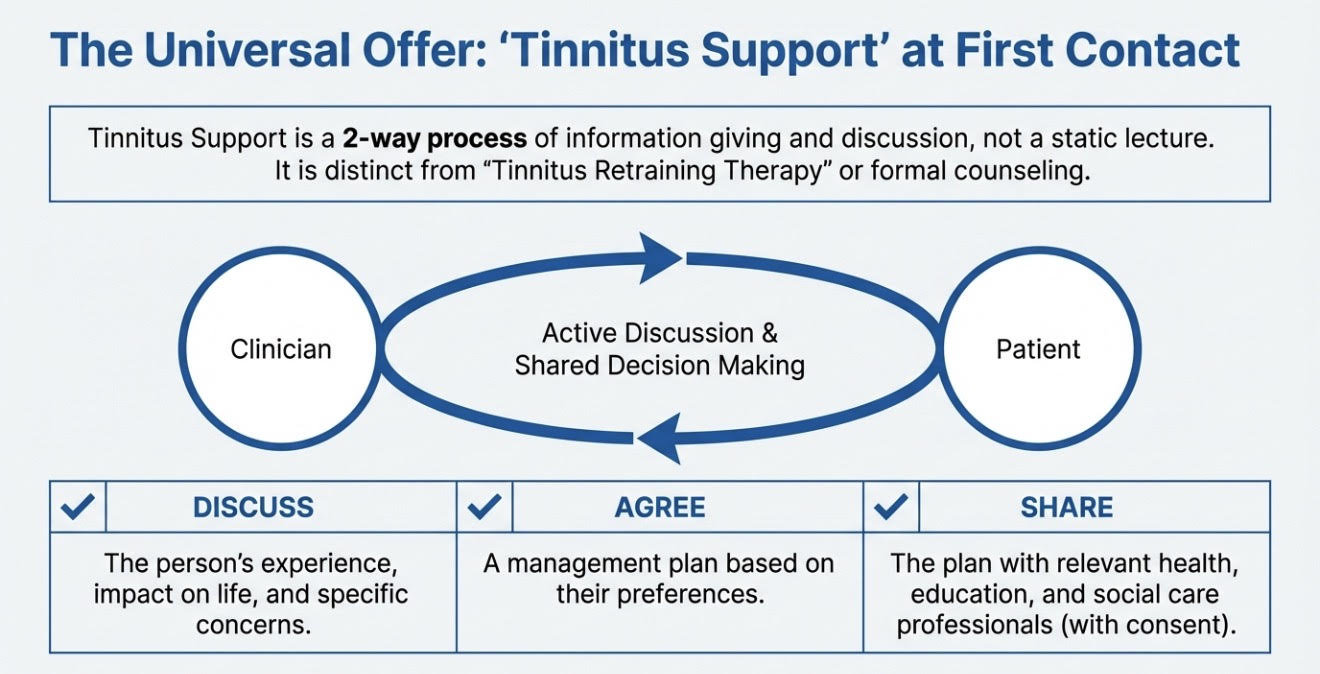
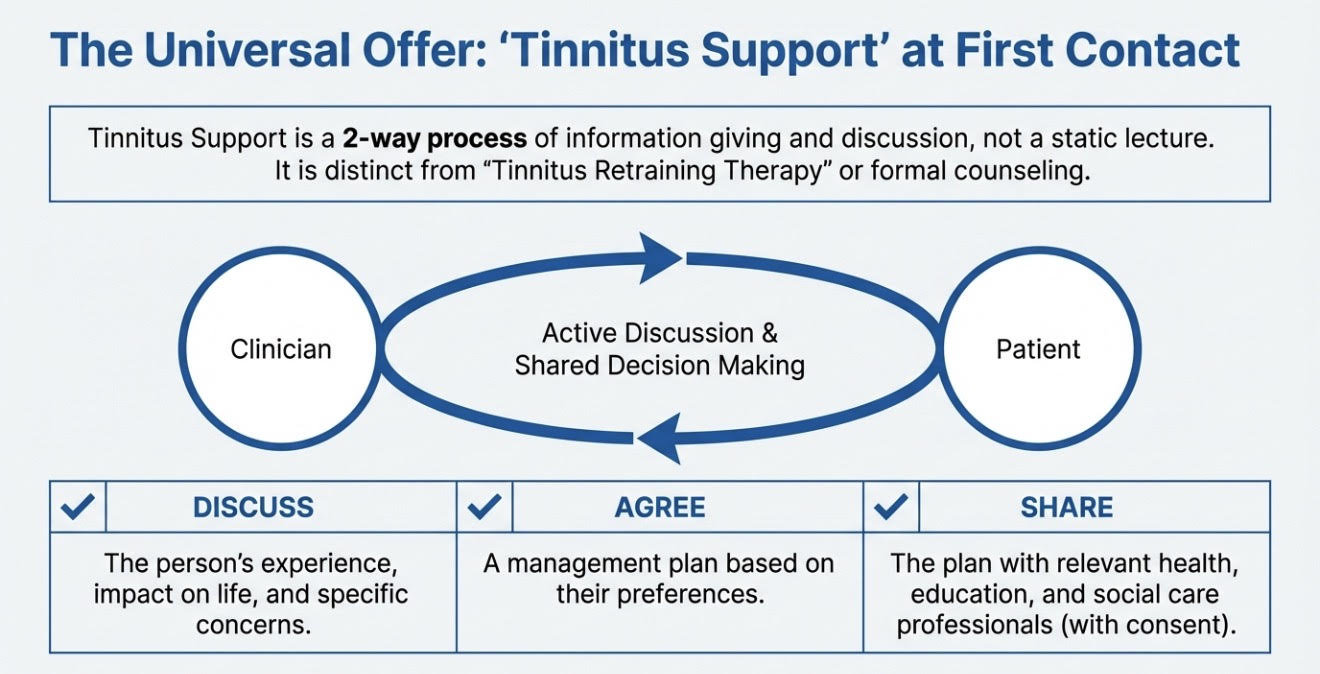
My first appointments are usually 90 minutes to two hours. The initial session focuses mainly on detailed informational counselling, careful fact-finding, and making a clear plan.
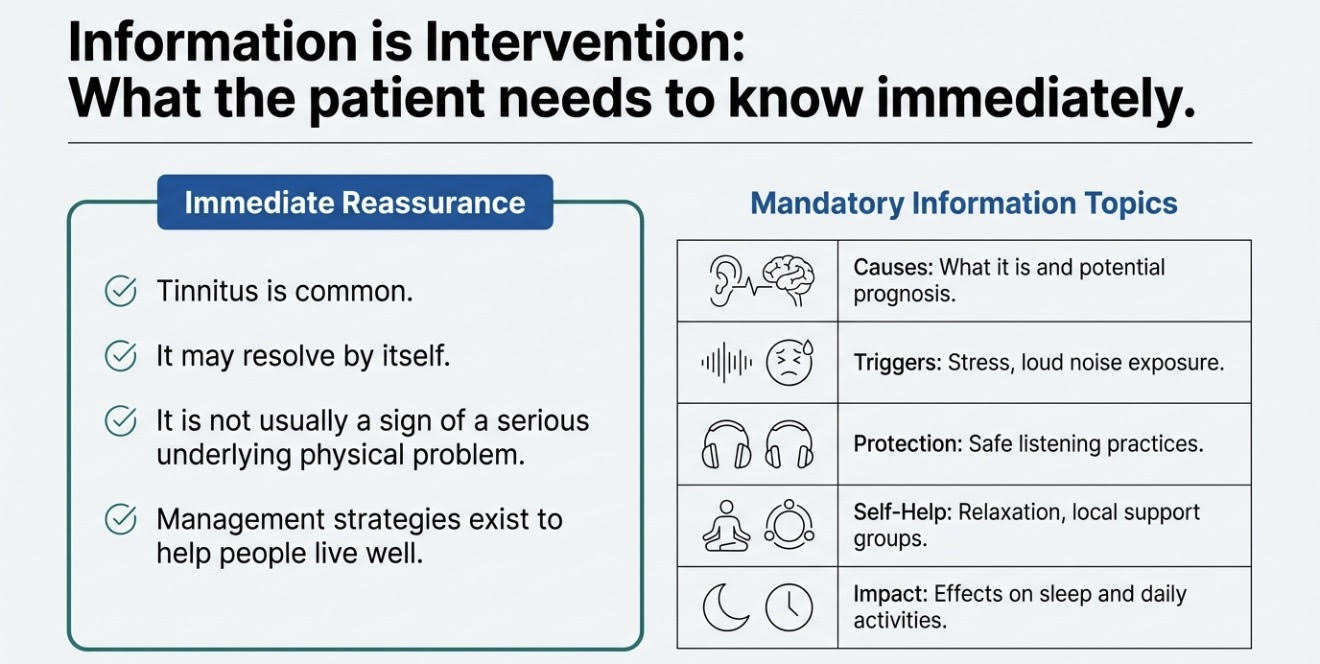
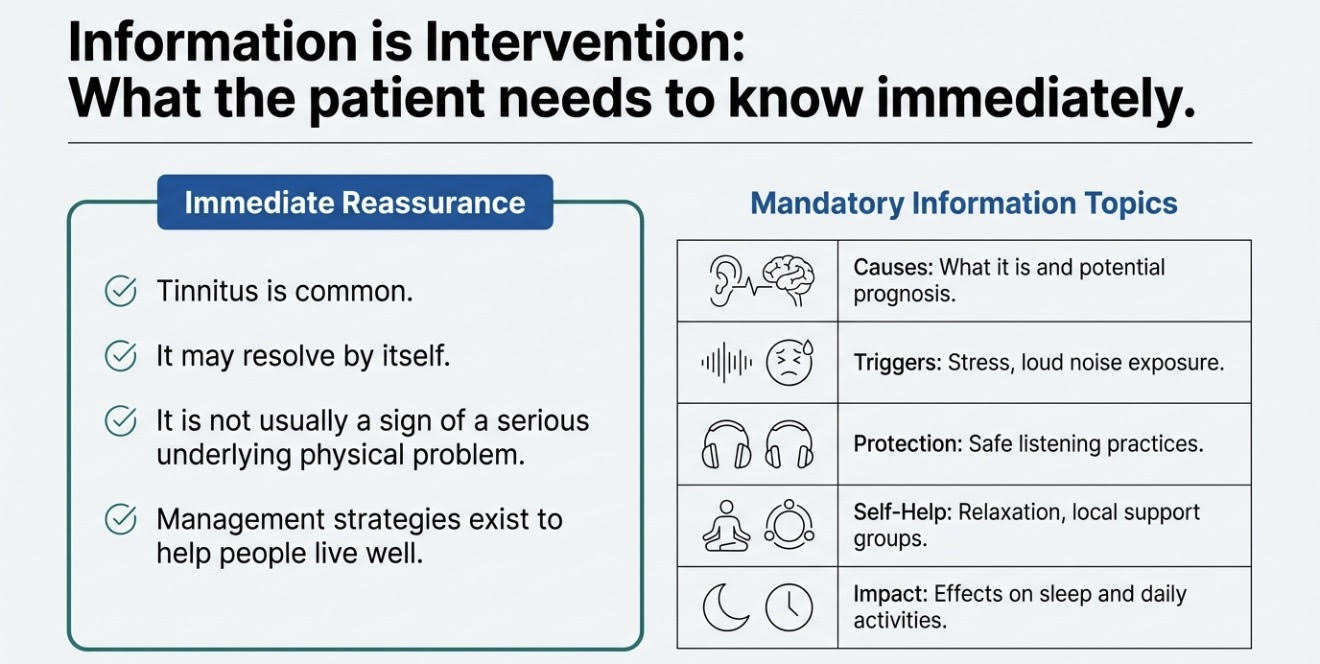
After our consultation, while we were writing notes, she spent about 15 minutes thanking me — simply for doing my job. I just presented her all the facts and some of the educated inferences from those facts, in a simplified and structured manner; so she could process it and understand it. I did not think it was an extraordinary piece of information that only I had access to. This information is very easily available to most health professionals. Lot of it is in NICE guidelines too. Still, she said this was the type of information she had been searching for online and during her initial appointments but had not received.
She left hopeful.
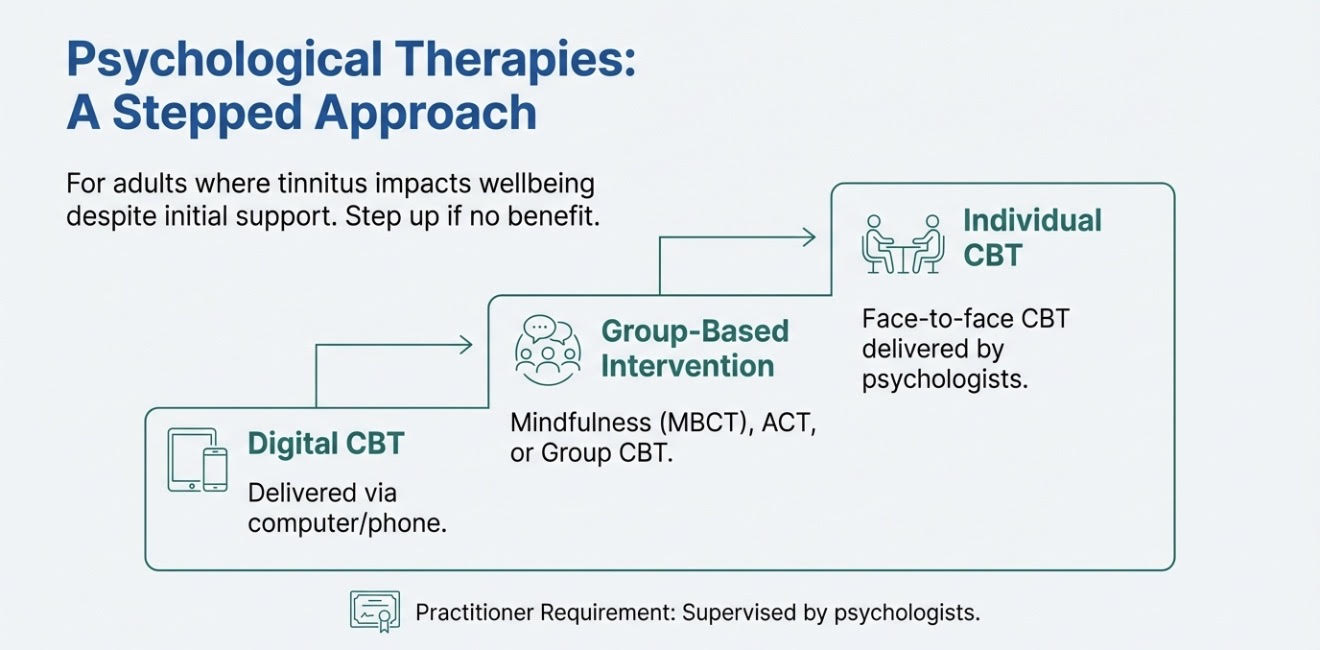
She now thinks that she understands much better what she needs to do in order to get her life back — in her words — because we have a plan. We have a solution that involves her and some tools and techniques. In fact, we have several solutions, including onward referral for a structured therapeutic approach. Now that she understands why a talking therapy approach may also be required, she is very open to it.
The point of sharing this, especially towards the end of Tinnitus Awareness Week, is that despite all the research in this specialist area and despite NICE guidance — which I have been posting about throughout the week on my Socials — there is still a lack of accurate information and a lot of misinformation at multiple contact points for people with bothersome tinnitus.
I hope that if this reaches even a handful of healthcare professionals, and perhaps some people living with tinnitus, they understand that “distract yourself” is not a management strategy. In fact, the last thing you want to do when lying in bed is try to force yourself to distract from tinnitus. That is not a technique.
If I ask you not to think about a monkey, what happens? You immediately think about monkeys. There have been classic psychology experiments where one group was told not to think about monkeys but to mention it if they did, and another group was told to think about monkeys and mention it when they did. The group told not to think about monkeys thought about them more.
The same principle applies here.
Suppression increases focus. Distraction can be one short-term coping tool. It is not a management plan. Especially in tinnitus, where:
- The brain’s threat response matters
- Emotional processing matters
- Understanding the mechanism reduces fear
- Validation is often the turning point
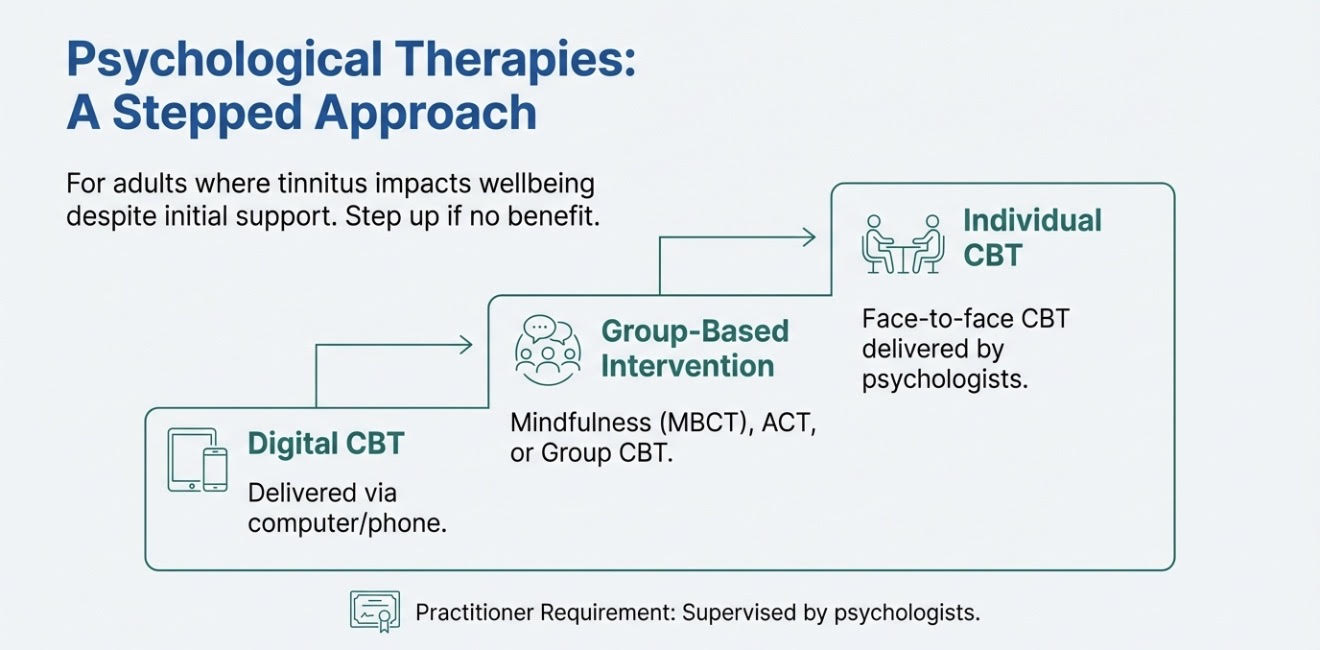
However, there are many ways to teach the brain and body to respond differently to tinnitus, but this requires structured practice and behavioural change. It is about retraining patterns and conditioning.
People don’t all learn — or cope — in the same way. Our values, beliefs, past experiences, and habits shape how we process information. Some people need logic. They want the mechanism explained so it makes sense. Others are comfortable trusting clinical expertise without needing every detail unpacked.
Some respond well to clear goals and measurable steps. Some need grounding, pacing, and nervous-system regulation first. Some are visual learners. Others connect through stories and lived examples.
Each to their own.
There isn’t one “right” way. There’s the right way for that person. Tinnitus management is no different. If the aim is to calm an overactive threat response within the auditory system, the approach has to be tailored. Humans may have evolved, but the primitive brain is still very much in charge when it comes to perceived threat. The sympathetic nervous system — that built-in alarm system — can be triggered by something as small as a passing comment from a colleague, a family member, even a stranger on the road. It doesn’t take much to flip the switch.
Tinnitus often gets pulled into that same alarm circuitry.
There are multiple evidence-based strategies that reduce distress and stop tinnitus from snowballing into a much larger problem. But they need to be applied with thought, structure, and clinical judgement — not handed out as generic advice.
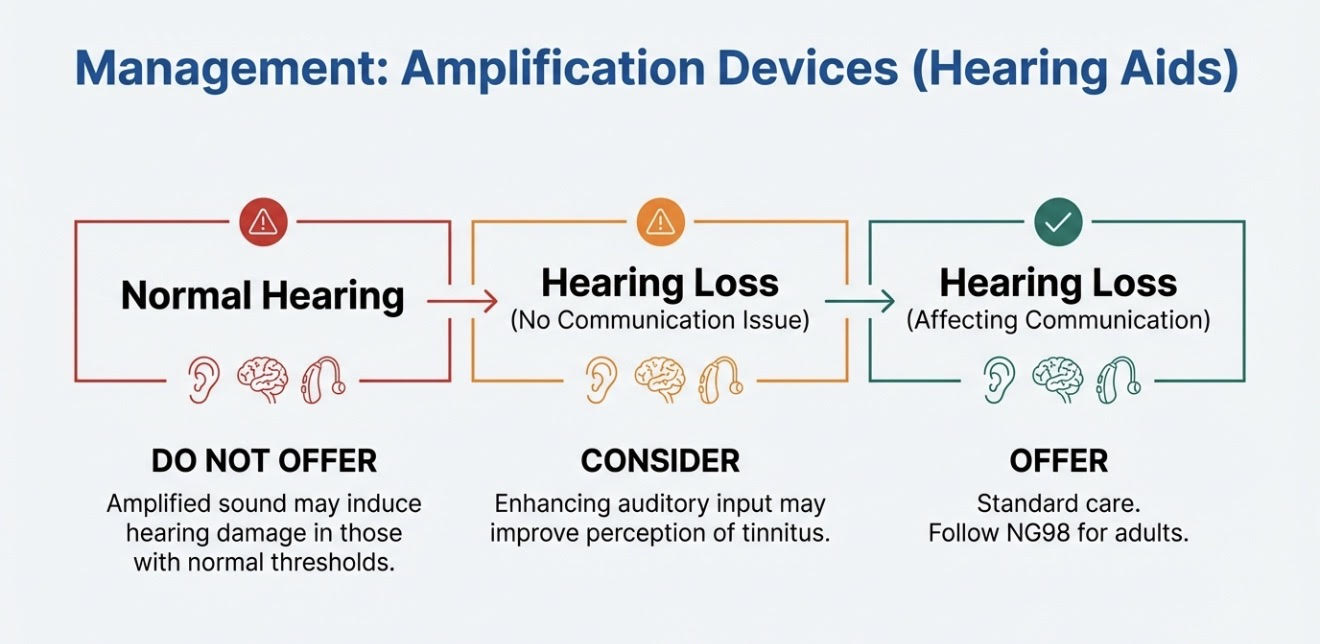
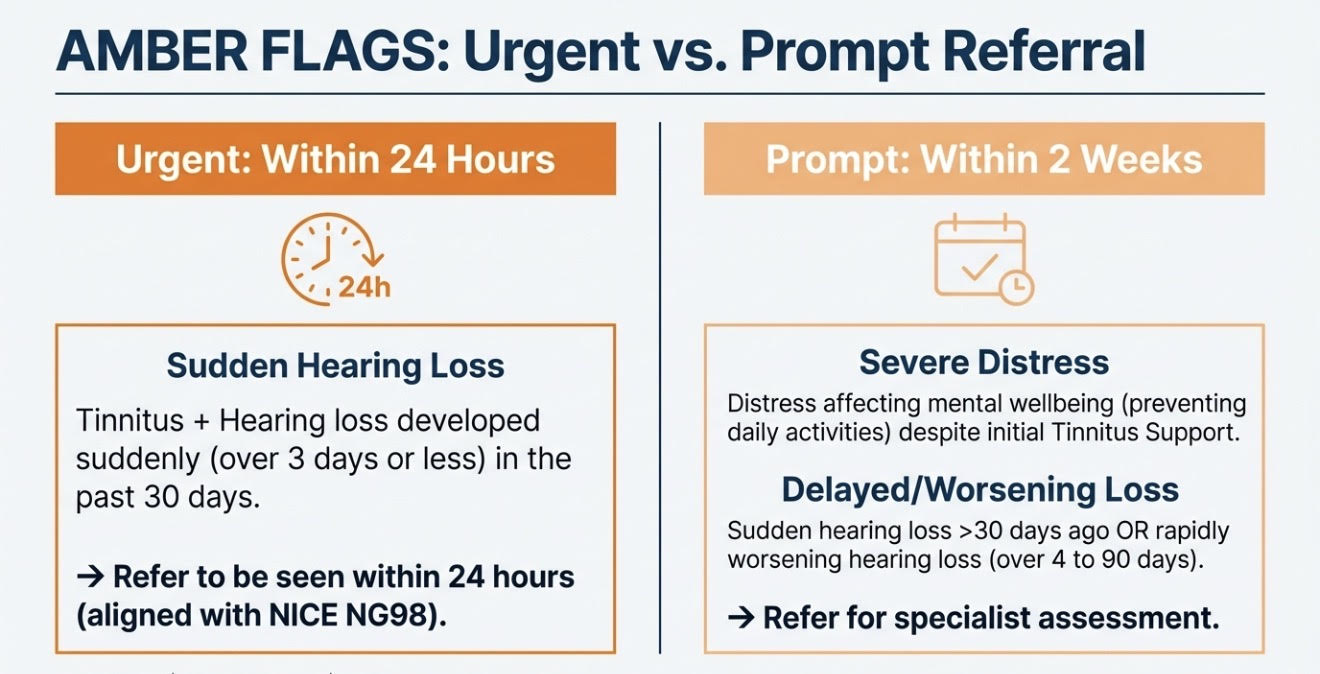
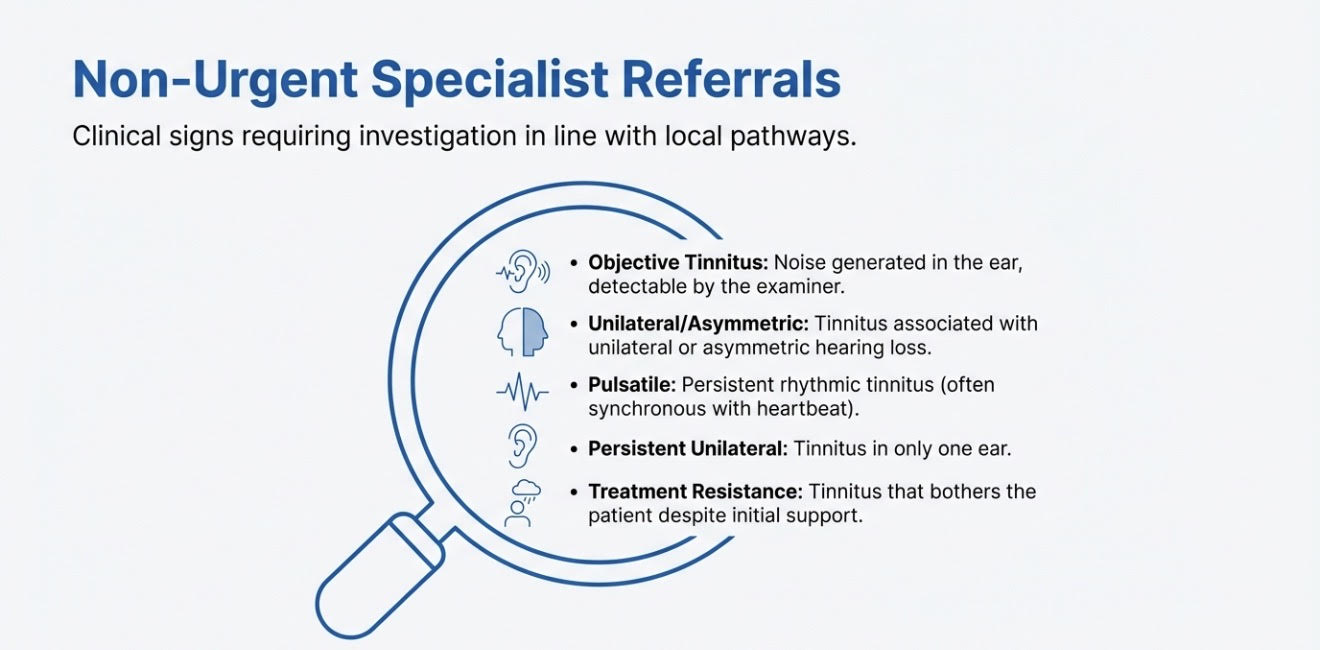
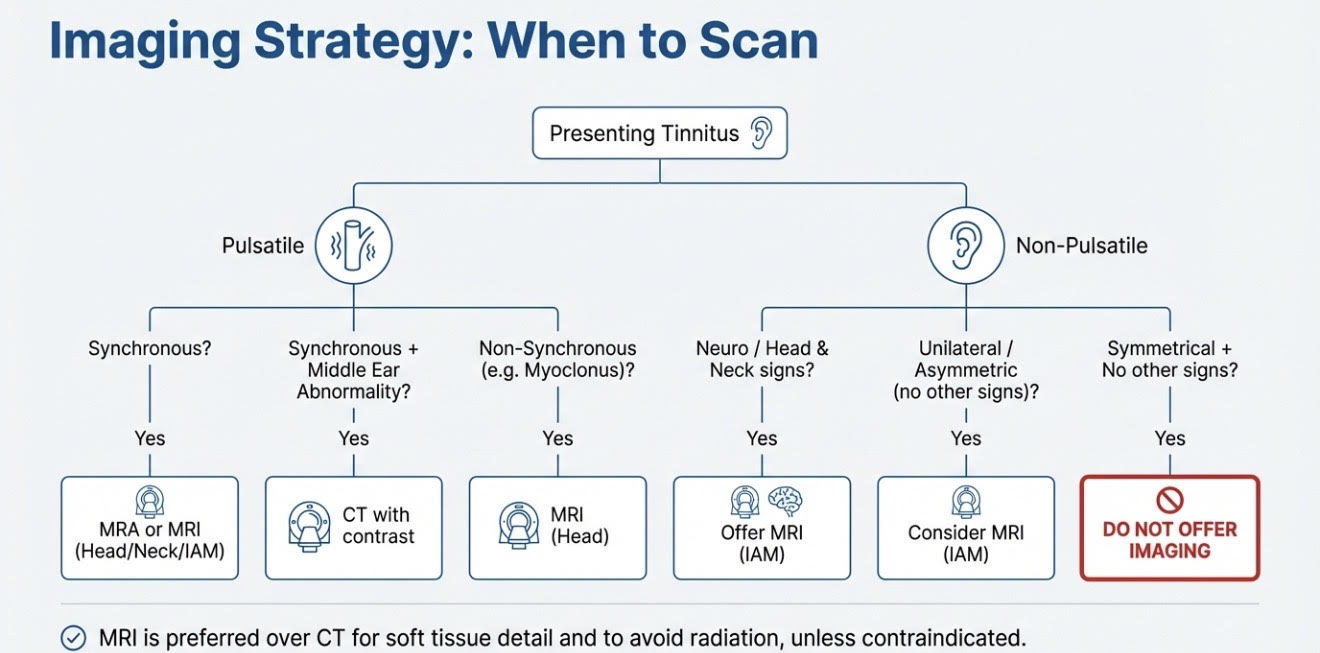
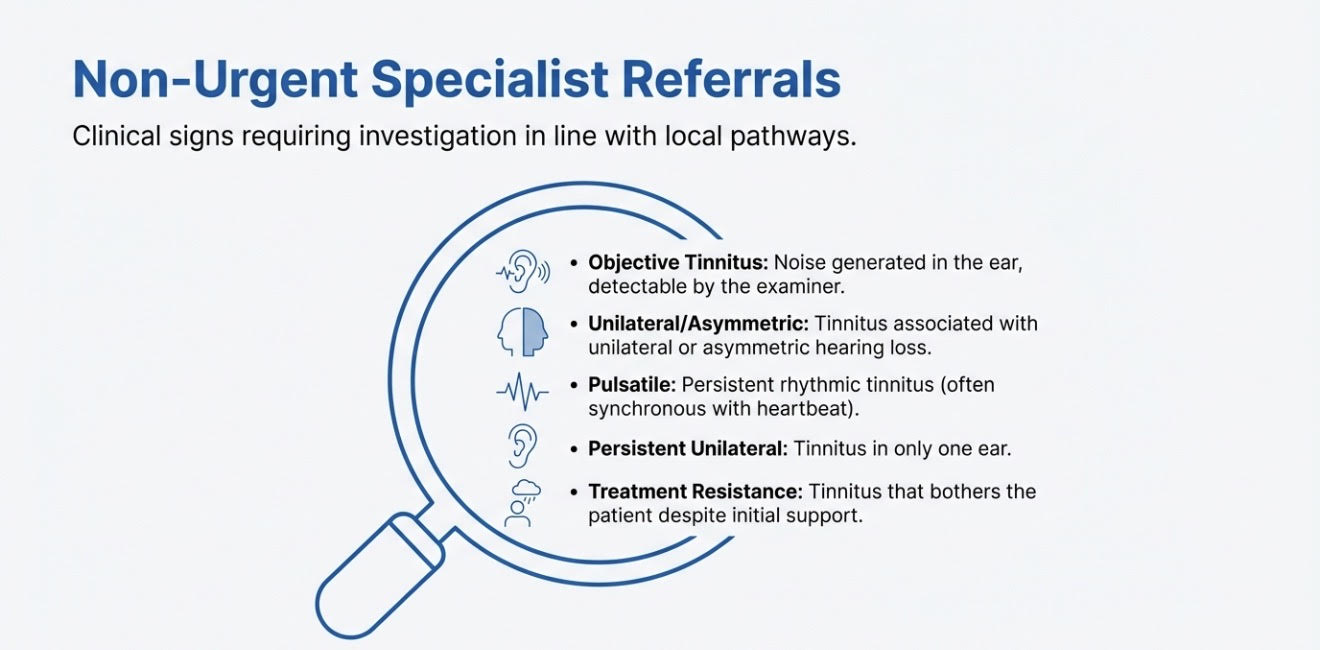
So my message to colleagues is straightforward: when you see someone with bothersome tinnitus, refer them to a clinician trained in tinnitus management. Leaflets and self-distraction often doesn’t help. Training the system must therefore be individualised. There are multiple evidence-based techniques to prevent tinnitus from becoming an even bigger problem. So, my appeal to all healthcare professionals reading this is simple:
I will end by thanking all the excellent ENT surgeons, Audio-Vestibular Physicians, primary care physicians, audiologists, hearing therapists, tinnitus specialists, psychologists, physiotherapists, Sector organisations and everyone else who work with people who have bothersome tinnitus and tinnitus management — whether individually or as part of multidisciplinary teams.
Done properly, this work is life-changing — for the people we help, and for us as clinicians striving to grow and practise at a higher level. This makes you a better part of your community and the world becomes a better place. If you are not in Kent or around, ask me to point you in the right direction to refer someone who has bothersome tinnitus.