Vestibular Migraine: Symptoms, Diagnosis and Treatment
Vestibular migraine (VM) is a dizziness condition that causes repeated, unprovoked attacks of dizziness, imbalance, motion sensitivity, and sometimes headaches.
It is one of the most common causes of recurrent vertigo, but is frequently missed or misdiagnosed as Ménière’s disease, anxiety, “ear problems”, or simply “stress”.
VM affects an estimated 3% of the population, but up to 30–50% of people diagnosed with migraine experience vestibular symptoms at some point. This is one of the most common diagnosis of dizziness along with BPPV and vestibular weakness. Research shows it is more common in women and often begins in middle adulthood, although it can occur at any age—even in children.
What Are the Main Symptoms of Vestibular Migraine?

Symptoms vary between individuals and even from attack to attack, but common features include:
Vestibular symptoms
- Spinning vertigo
- Rocking / Swaying sensation
- Imbalance or unsteady gait
- Motion sensitivity (car, supermarket aisles, scrolling screens)
Sensory symptoms
- Sensitivity to light, sound, or smells
- Vision changes (blur, after-images, visual “snow”)
Headache symptoms
- Throbbing pain (but headache is not always present)
- Pain on one side of the head
- Worsening with physical activity
Cognitive / Emotional effects
- Brain fog
- Anxiety during or after attacks
Attacks can last minutes, hours, or days.
What Causes Vestibular Migraine?

The exact mechanism is complicated and still being studied, but involves abnormal processing in:
- The brain (brainstem and vestibular nuclei)
- Visual–vestibular pathways
- Pain modulation networks
Genetic predisposition and environmental triggers are involved.
Vestibular migraine is not a problem of the ear itself, despite the dizziness.
How is Vestibular Migraine Diagnosed?
Diagnosis is clinical. There is no single test that “proves” vestibular migraine. It is a diagnosis of exclusion, where a complete vestibular investigation is performed to rule out a significant vestibular weakness before relating the symptoms—including dizziness and balance problems—to the diagnosis of vestibular migraine.
Vestibular testing (VNG, vHIT, VEMP, audiometry) is often normal, but used to rule out:
- Ménière’s disease
- BPPV
- Vestibular neuritis
- Central pathologies
Lab tests and MRI are used when symptoms are atypical.
Common Triggers of Vestibular Migraine
Triggers are highly individual, but frequently reported ones include:
Diet
- Caffeine
- Alcohol (especially red wine)
- Aged cheese
- Processed meats
- MSG / Aspartame
- Fasting / irregular meals
Lifestyle
- Poor sleep
- Dehydration
- High stress
- Bright / Flickering lights
- Motion and busy visual environments
Hormonal
- Menstruation
- Hormone therapy changes
Sensory overload
- Loud noise
- Screen scrolling
Treatment Options for Vestibular Migraine
There is no particular cure just as general migraine, but most people improve with a combination of:
1. Lifestyle and Trigger Management

Often the most effective approach:
- Regular meals
- Adequate hydration
- Reduction of caffeine and alcohol
- Sleep routine
- Stress management
Not everyone needs a strict diet, but identifying personal triggers is crucial.
2. Preventive Medications

Used for frequent or severe attacks and prescribed by a medical doctor:
- Amitriptyline
- Nortriptyline
- Propranolol
- Topiramate
- Candesartan
- Venlafaxine
Response may take 6–12 weeks.
3. Acute Medications

To treat attacks, your medical team may prescribe:
- Triptans
- NSAIDs
- Antiemetics
Effectiveness varies.
4. Vestibular Rehabilitation Therapy (VRT)

Not “balance exercises” in a casual sense.
Useful for:
- Motion sensitivity
- Balance impairment
- Visual–vestibular mismatch
Evidence suggests Vestibular Rehabilitation Therapy (VRT) helps, especially when combined with migraine control.
5. Nutritional Supplements

Evidence is limited but some data supports:
- Magnesium
- Riboflavin (B2)
- CoQ10
Low risk, but take these only after consulting a doctor.
Prognosis- long term outcome of vestibular migraine
Vestibular migraine is chronic but manageable.
Most patients achieve substantial improvement with a personalised plan.
The biggest risk factor for persistent symptoms?
Doing nothing and hoping it goes away.
Vestibular Migraine vs Ménière’s Disease
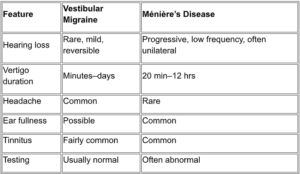
It is possible to have both conditions, which complicates diagnosis.
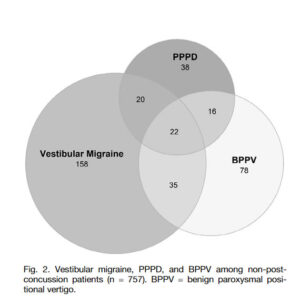
Other common overlaps
VM with persistent perceptual postural dizziness (PPPD) and BPPV
Data Credit: https://dizziness-and-balance.com/disorders/central/migraine/mav.html?JAVASCRIPT=ON
Scientific References
Bárány Society / ICHD
Lempert, T., & von Brevern, M. (2019). Vestibular migraine. Neurologic Clinics.
https://pubmed.ncbi.nlm.nih.gov/31563227/
Epidemiology & diagnosis
Formeister, E. J., Rizk, H. G., Kohn, M. A., & Sharon, J. D. (2018). The epidemiology of vestibular migraine: A population-based survey study. Otolaryngology–Head and Neck Surgery, 39(8), 1037–1044. https://doi.org/10.1097/MAO.0000000000001900
Clinical aspects and pathophysiology
Furman, J. M., Marcus, D. A., & Balaban, C. D. (2013). Vestibular migraine: Clinical aspects and pathophysiology. The Lancet Neurology, 12(7), 706–715. https://doi.org/10.1016/S1474-4422(13)70107-8
Treatment
Smyth, D., Britton, Z., Murdin, L., Arshad, Q., & Kaski, D. (2022). Vestibular migraine treatment: A comprehensive practical review. Brain, 145(11), 3741–3754. https://doi.org/10.1093/brain/awac264
VRT
Whitney, S. L., Alghwiri, A. A., & Alghadir, A. (2016). An overview of vestibular rehabilitation. Handbook of Clinical Neurology, 137, 187–205. https://doi.org/10.1016/B978-0-444-63437-5.00013-3
Dietary triggers
Hindiyeh, N. A., Zhang, N., Farrar, M., Banerjee, P., Lombard, L., & Aurora, S. K. (2020). The role of diet and nutrition in migraine triggers and treatment: A systematic literature review. Headache, 60(7), 1300–1316. https://doi.org/10.1111/head.13836
Vestibular Migraine FAQ
Q.1. Is vestibular migraine dangerous?
No, but it is disruptive and disabling. Symptoms are real, not psychological.
Q.2. Do I need a brain scan?
Sometimes, especially if symptoms are new, sudden or atypical.
Q.3. Is it caused by anxiety?
No. Anxiety can worsen symptoms, but it does not cause them.
Q.4. Will I go deaf?
Unlikely. VM rarely causes permanent hearing loss.
Q.5. Does vestibular rehab help?
Yes, especially for motion sensitivity and imbalance.
Q.6. Do I need medication?
Not always. Lifestyle strategy alone works for many patients.
Q.7. Is caffeine bad?
For many people, yes—although not universally.
Q.8. Can children get it?
Yes, but often misdiagnosed as “motion sickness”.
Key Takeaway
Vestibular migraine is common, real, and treatable.
A combination of lifestyle modification, medical treatment, and vestibular rehabilitation is usually effective.
The goal is not perfection—just control good enough to get your life back.